- Ventricular-Assist Devices Overview: What They Are and Why They Matter
- How Ventricular-Assist Devices Support Heart Disease Patients
- Real-Life Examples of Ventricular-Assist Device Impact
- Key Benefits and Potential Challenges of Ventricular-Assist Devices
- Recommendations for Patients Using Ventricular-Assist Devices
1. Ventricular-Assist Devices Overview: What They Are and Why They Matter
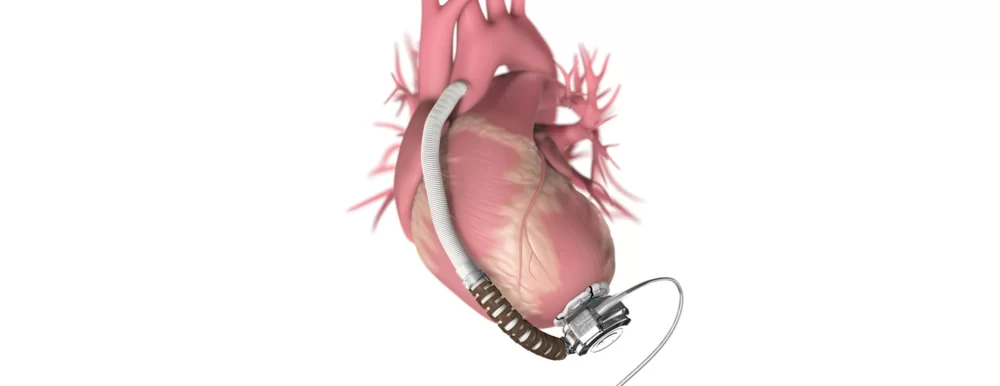
Heart disease remains one of the leading causes of mortality worldwide, especially when it progresses to severe heart failure. In such cases, ventricular assist devices (VADs) have emerged as a groundbreaking mechanical support option. A ventricular assist device is a small, mechanical pump implanted in the body to help the weakened heart ventricles pump blood more effectively.
Unlike traditional medications or lifestyle changes that primarily manage symptoms, VADs provide direct mechanical circulatory support, offering a lifeline for patients whose hearts struggle to maintain adequate blood flow. These devices can serve as a bridge to heart transplantation or, in some cases, as a long-term therapy known as destination therapy.

1.1 Types of Ventricular-Assist Devices
There are several types of VADs, typically categorized based on which heart chamber they support. Left ventricular assist devices (LVADs) are the most common, assisting the left ventricle which pumps oxygenated blood to the entire body. Right ventricular assist devices (RVADs) and biventricular assist devices (BiVADs) support the right ventricle or both ventricles, respectively, depending on the patient's condition.
Atlanta Heart Specialists
atlanta heart specialists
4375 Johns Creek Pkwy #350, Suwanee, GA 30024, USA

1.2 The Evolution of VAD Technology
The development of ventricular assist devices has advanced rapidly over recent decades. Early bulky, external pumps have evolved into smaller, more durable, and increasingly implantable devices with improved battery life and control systems. These innovations have made VADs more accessible and safer for a wider range of patients.
2. How Ventricular-Assist Devices Support Heart Disease Patients
In patients with advanced heart failure, the heart muscle weakens to the point it cannot supply enough blood to meet the body's demands. This can lead to fatigue, shortness of breath, fluid retention, and ultimately life-threatening complications. Ventricular assist devices step in by mechanically taking over part or all of the heart's pumping function.
2.1 Physiological Impact of VADs
By improving cardiac output, VADs help relieve symptoms and improve organ function. The heart muscle can sometimes recover due to reduced workload, and patients experience enhanced quality of life and longer survival. VADs also stabilize patients awaiting heart transplantation, reducing the risk of complications during the waiting period.
2.2 Integration with Medical Therapy
VAD therapy does not replace medical treatment but complements it. Patients continue receiving medications, lifestyle counseling, and regular monitoring. Coordination between cardiologists, surgeons, and specialized VAD teams is critical to optimize patient outcomes.
3. Real-Life Examples of Ventricular-Assist Device Impact
Consider the story of Michael, a 58-year-old man diagnosed with end-stage heart failure due to ischemic cardiomyopathy. Michael’s symptoms were debilitating, and he was listed for a heart transplant. To bridge the gap, surgeons implanted a left ventricular assist device. Within weeks, Michael noticed remarkable improvements: his energy returned, he could walk his dog again, and his hospitalizations decreased significantly.
Michael’s case reflects how VADs can restore hope and provide practical support during critical periods. Stories like his inspire many patients to consider this life-saving technology.
3.1 Notable Medical Cases and Research Findings
Clinical studies consistently show that VAD recipients experience significant symptom relief and increased survival rates compared to those on medical therapy alone. One landmark trial demonstrated a 70% survival rate at two years post-implant, compared to only 30% with medication management, emphasizing the transformative potential of ventricular assist devices.
4. Key Benefits and Potential Challenges of Ventricular-Assist Devices
VADs offer several undeniable benefits but also pose challenges that patients and caregivers must understand.
4.1 Benefits
Besides improving survival and quality of life, VADs enable patients to regain independence and reduce hospital stays. Modern devices come with sophisticated monitoring systems, allowing timely intervention if complications arise.
4.2 Challenges
Possible complications include infection, blood clots, and device malfunction. Patients require careful management of anticoagulation therapy and must adapt to living with an external controller and power source. Psychological adjustment to having a mechanical device implanted is also significant and requires support.
5. Recommendations for Patients Using Ventricular-Assist Devices
For those considering or living with a ventricular assist device, expert guidance is crucial. Regular follow-up visits, adherence to medication, and lifestyle modifications such as a heart-healthy diet and avoiding strenuous activities are essential.
Additionally, emotional and social support improves overall well-being. Support groups and counseling can help patients and families cope with the complexities of VAD therapy.
If you are seeking trusted information, quality devices, or support services tailored to ventricular assist device users, HeartCare Hub is a valuable resource. It offers access to specialized products, healthcare providers, and community networks dedicated to enhancing heart disease care.




















Deborah Heart and Lung Center
deborah heart and lung center
200 Trenton Rd, Browns Mills, NJ 08015, USA