Exploring Cardiomyopathy: What It Means, Who’s at Risk & What You Can Do
1. What is Cardiomyopathy?
Cardiomyopathy is a disease of the heart muscle that makes it harder for your heart to pump blood. This can lead to heart failure, a condition where the heart isn’t able to pump enough oxygen-rich blood to meet your body’s needs. Cardiomyopathy can develop over time and may result in complications such as arrhythmias (irregular heartbeats) or blood clots.
There are several types of cardiomyopathy, each with different causes and effects. The most common types include:
- Dilated Cardiomyopathy: The heart chambers enlarge, weakening the heart muscle and impairing its ability to pump blood.
- Hypertrophic Cardiomyopathy: The heart muscle becomes abnormally thick, making it difficult for the heart to pump blood effectively.
- Restrictive Cardiomyopathy: The walls of the heart become stiff, restricting the heart’s ability to fill with blood.
- Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC): A rare condition where fatty or fibrous tissue replaces the muscle in the right ventricle, which can lead to arrhythmias.
2. Who’s at Risk for Cardiomyopathy?
While cardiomyopathy can affect anyone, certain factors can increase the risk of developing this condition. These include:
- Family history: Cardiomyopathy can be inherited, meaning that if a close family member has the condition, you may be at higher risk.
- Age: Cardiomyopathy can occur at any age, but it is most common in people between 20 and 60 years old.
- High blood pressure: Chronic high blood pressure increases the risk of developing cardiomyopathy by putting added strain on the heart muscle.
- Heart attack: A previous heart attack can damage the heart muscle, leading to the development of cardiomyopathy.
- Other conditions: Diseases such as diabetes, thyroid disorders, and obesity can contribute to the risk of developing cardiomyopathy.
- Excessive alcohol use: Heavy drinking over time can lead to alcohol-induced cardiomyopathy.
3. Symptoms of Cardiomyopathy
The symptoms of cardiomyopathy vary depending on the type of condition and its severity. Early stages may not show clear symptoms, but as the disease progresses, you may experience:
- Shortness of breath: Difficulty breathing, especially during physical activity or while lying down.
- Fatigue: Feeling unusually tired or weak due to the heart’s inability to pump enough blood.
- Swelling: Fluid buildup in the legs, ankles, feet, or abdomen, causing swelling.
- Irregular heartbeats: Palpitations or arrhythmias can be felt as fluttering or rapid heartbeats.
- Chest pain: Some individuals with cardiomyopathy may experience chest discomfort, particularly during physical exertion.
4. Causes of Cardiomyopathy
Cardiomyopathy can be caused by a variety of factors, including genetic inheritance, lifestyle choices, and other underlying medical conditions. Some of the common causes include:
- Genetic factors: Inherited forms of cardiomyopathy are passed down from one generation to the next, often affecting multiple family members.
- High blood pressure: Long-term high blood pressure can lead to thickening and stiffening of the heart muscle.
- Coronary artery disease: Blockages in the heart’s arteries can reduce blood flow, causing damage to the heart muscle.
- Viral infections: Some viral infections can cause inflammation of the heart muscle, leading to cardiomyopathy.
- Drugs and toxins: Long-term use of certain drugs (such as chemotherapy drugs) and alcohol can lead to the development of cardiomyopathy.
5. How to Prevent and Manage Cardiomyopathy
While it may not be possible to prevent cardiomyopathy in all cases, there are steps you can take to reduce your risk and manage the condition if you are diagnosed:
- Maintain a healthy weight: Losing excess weight can reduce the strain on your heart and lower your risk of developing heart disease.
- Eat a balanced diet: Eating heart-healthy foods such as fruits, vegetables, whole grains, and lean proteins can help protect your heart.
- Exercise regularly: Moderate exercise can help strengthen the heart and improve circulation. However, it is essential to talk to your doctor before starting any exercise regimen.
- Limit alcohol consumption: Drinking alcohol in moderation or abstaining altogether can prevent alcohol-induced cardiomyopathy.
- Manage blood pressure: Regularly monitor and manage high blood pressure with lifestyle changes or medications as needed.
- Take prescribed medications: Medications such as beta-blockers, ACE inhibitors, or diuretics may be prescribed to help manage symptoms and prevent complications.
6. Treatment for Cardiomyopathy
The treatment for cardiomyopathy depends on the type and severity of the condition. Options may include:
- Medications: To control symptoms, manage heart failure, and prevent arrhythmias.
- Implantable devices: Devices such as pacemakers or defibrillators may be implanted to help regulate heart rhythms.
- Surgery: In some cases, surgery may be needed to repair damaged heart tissue, correct valve issues, or even replace the heart with a transplant.
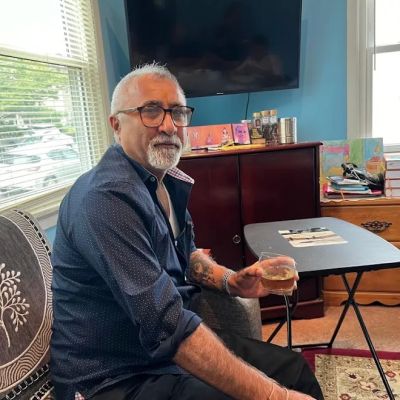
7. Real-Life Case Study: John’s Battle with Cardiomyopathy
John, a 58-year-old man, was diagnosed with dilated cardiomyopathy after experiencing shortness of breath and swelling in his legs. His family history of heart disease and high blood pressure made him more susceptible to the condition. After undergoing several tests, John’s doctor prescribed medications to help reduce fluid buildup and control his heart’s rhythm. With a combination of lifestyle changes, including weight loss, exercise, and reduced alcohol intake, John was able to stabilize his condition and significantly improve his quality of life.
8. Conclusion: Managing Cardiomyopathy for a Healthier Life
Cardiomyopathy is a serious condition, but with early diagnosis and proper management, many people with cardiomyopathy can lead fulfilling lives. If you suspect you are at risk or have been diagnosed with cardiomyopathy, make sure to work closely with your healthcare provider to find the best treatment options for you.
For more heart health resources and services, visit HeartCare Hub to find expert advice tailored to your needs.