- what-is-cardiomyopathy-and-why-it-matters
- different-types-of-cardiomyopathy-and-how-they-develop
- the-real-life-impact-of-a-weakened-heart-muscle
- early-warning-signs-and-diagnostic-methods
- treatment-options-lifestyle-and-medical-approaches
- living-well-with-cardiomyopathy-personal-strategies
1. What Is Cardiomyopathy and Why It Matters
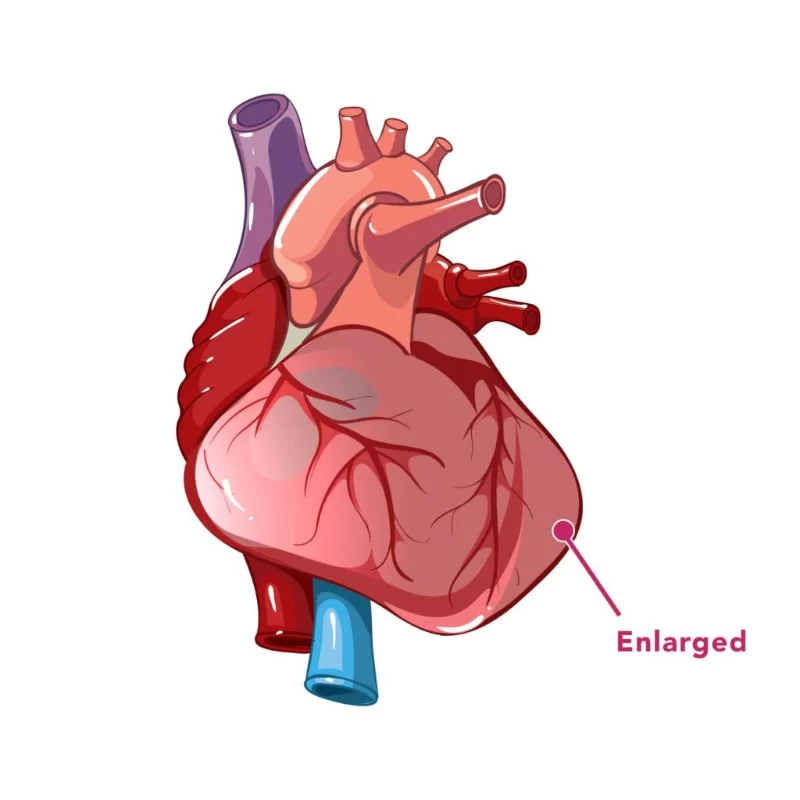
Cardiomyopathy is a condition where the heart muscle becomes weakened, stiff, or structurally abnormal, making it harder for the heart to pump blood effectively. Unlike typical heart disease caused by blocked arteries, cardiomyopathy often affects the entire heart muscle itself. Over time, this condition may lead to congestive heart failure, life-threatening arrhythmias, or even sudden cardiac arrest if left untreated.
Understanding cardiomyopathy is especially important in the U.S., where millions live with undiagnosed or misdiagnosed heart muscle conditions. The more we know about early symptoms and progression, the better we can manage it—and live longer, fuller lives. At HeartCare Hub, we believe awareness is the first step to action.

2. Different Types of Cardiomyopathy and How They Develop
2.1. Dilated Cardiomyopathy (DCM)
This is the most common form of cardiomyopathy. The heart's chambers—especially the left ventricle—enlarge and become weaker. Often linked to genetic factors, alcohol abuse, or viral infections, DCM reduces the heart's ability to pump blood, which can result in fatigue, breathlessness, and swelling in the limbs.
Atlanta Heart Specialists
atlanta heart specialists
4375 Johns Creek Pkwy #350, Suwanee, GA 30024, USA

2.2. Hypertrophic Cardiomyopathy (HCM)
HCM involves abnormal thickening of the heart muscle, particularly the septum (wall between the ventricles), which can obstruct blood flow. It's often inherited and may go undetected until a stressful episode or sudden cardiac event. Many athletes who collapse during games are later found to have HCM, highlighting its silent danger.
2.3. Restrictive Cardiomyopathy
This rare form causes the heart walls to become stiff, limiting their ability to expand and fill with blood. It may stem from diseases like amyloidosis or radiation exposure. Though it’s rare, it often presents severe symptoms and has limited treatment options.
2.4. Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)
ARVC replaces healthy heart muscle with scar tissue and fat, mostly affecting the right ventricle. This disrupts the heart's rhythm and can lead to dangerous arrhythmias. It’s typically genetic and often first noticed in young adults or athletes.
3. The Real-Life Impact of a Weakened Heart Muscle
Imagine being 45, physically active, and suddenly finding yourself out of breath walking up stairs. That was the reality for Michael, a Houston-based chef. After weeks of worsening fatigue, he was diagnosed with dilated cardiomyopathy. “I thought I was just overworked,” he said, “but my heart was failing.”
For Michael, this meant major lifestyle changes—less caffeine, no alcohol, and a strict medication routine. But it also meant gaining control over his life again. With the support of HeartCare Hub and a cardiologist who explained his condition in detail, Michael returned to his kitchen six months later—with a pacemaker and a renewed appreciation for life.
4. Early Warning Signs and Diagnostic Methods
4.1. Common Symptoms
Signs of cardiomyopathy can be subtle or mimic other conditions. These include:
- Persistent fatigue
- Shortness of breath, even at rest
- Swelling in ankles, feet, or legs
- Irregular heartbeat or palpitations
- Chest discomfort
4.2. Diagnostic Tools
Cardiologists often use a combination of tests to detect cardiomyopathy. These include:
- Echocardiogram: Offers real-time imaging of heart structure and function
- Electrocardiogram (ECG): Tracks electrical signals and rhythm abnormalities
- Cardiac MRI: Provides detailed imaging of heart tissue
- Genetic testing: Especially for those with a family history of cardiomyopathy
5. Treatment Options: Lifestyle and Medical Approaches
5.1. Medications
Patients are often prescribed beta-blockers, ACE inhibitors, or diuretics to reduce strain on the heart. For those with arrhythmias, anticoagulants or rhythm control drugs may also be necessary.
5.2. Lifestyle Adjustments
Quitting smoking, eating a heart-healthy diet, reducing sodium intake, and managing stress are all part of a strong defense plan. Regular—but gentle—exercise is encouraged under medical supervision.
5.3. Devices and Surgical Options
Some patients benefit from implanted devices like pacemakers or ICDs (Implantable Cardioverter Defibrillators) to regulate rhythm or prevent sudden cardiac death. In severe cases, a heart transplant may be considered.
6. Living Well with Cardiomyopathy: Personal Strategies
6.1. Mental Health Matters
Dealing with a chronic condition affects more than your body. Many patients experience anxiety or depression. Support groups and counseling can help you stay mentally strong. Seeking communities through platforms like HeartCare Hub can connect patients and caregivers alike.
6.2. Building a Care Team
Managing cardiomyopathy isn’t a solo journey. It involves cardiologists, dietitians, physical therapists, and sometimes even genetic counselors. Having a responsive care team is crucial for navigating the ups and downs of the condition.
6.3. Regular Monitoring and Hope
Regular follow-ups, medication reviews, and imaging tests ensure your condition stays stable or improves. And with advancements in genetic therapies and personalized medicine, the future is becoming brighter for those with cardiomyopathy.




















Deborah Heart and Lung Center
deborah heart and lung center
200 Trenton Rd, Browns Mills, NJ 08015, USA