- Why Hydration Matters for Heart Health
- How Water Intake Affects Cardiovascular Function
- Hydration’s Impact on Common Heart Disease Factors
- Real-Life Stories Demonstrating Hydration’s Role in Heart Disease
- Tips to Maintain Adequate Hydration for Heart Health
- Resources from HeartCare Hub for Heart-Healthy Hydration
1. Why Hydration Matters for Heart Health
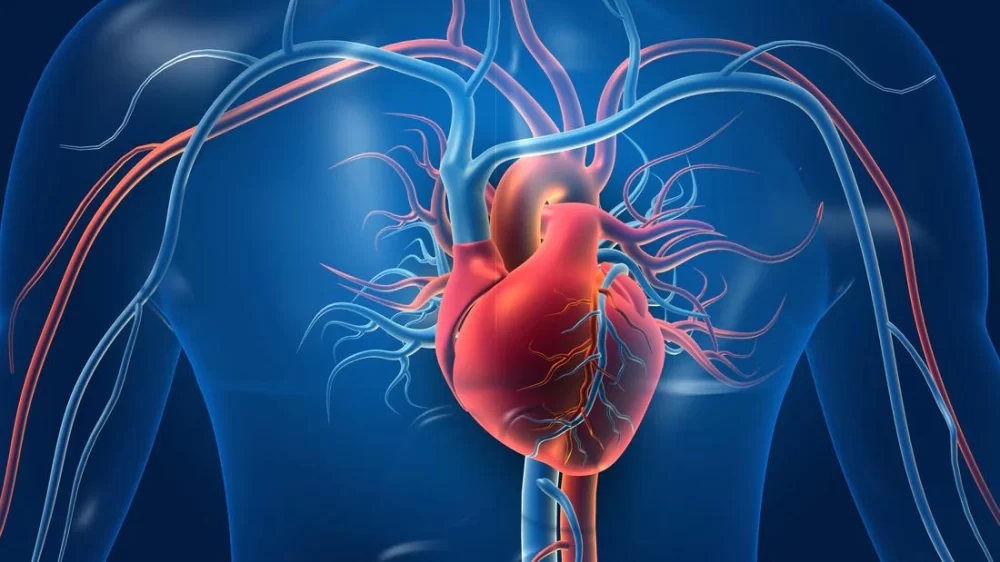
Maintaining proper hydration is often overlooked in discussions about heart disease, yet it plays a fundamental role in supporting cardiovascular function. The human body is approximately 60% water, and the heart relies heavily on adequate fluid balance to pump blood efficiently. Dehydration thickens the blood, making it harder for the heart to circulate oxygen and nutrients to vital organs. Over time, this added strain can contribute to increased blood pressure and heart disease risk.
Hydration is more than just quenching thirst; it is essential for maintaining blood volume, regulating body temperature, and ensuring smooth blood flow. Understanding the importance of hydration helps us appreciate its preventive potential in heart disease management.

2. How Water Intake Affects Cardiovascular Function
The cardiovascular system depends on a well-hydrated blood supply to function optimally. Water facilitates the transport of electrolytes like potassium and sodium, which are critical for regulating heartbeat and muscle contractions. When hydration levels drop, electrolyte imbalances can occur, potentially causing arrhythmias or irregular heartbeats.
Capital Health Medical Center – Hopewell
capital health medical center hopewell
1 Capital Way, Pennington, NJ 08534, USA

2.1 Blood Viscosity and Heart Workload
When dehydrated, blood becomes more viscous, increasing resistance in blood vessels. The heart must work harder to pump this thicker blood, raising heart rate and blood pressure. For individuals with existing heart conditions, this additional workload can exacerbate symptoms and lead to complications.
2.2 Temperature Regulation and Cardiovascular Stress
Hydration also influences the body’s ability to regulate temperature through sweating. Inadequate water intake limits heat dissipation, causing overheating that stresses the cardiovascular system. This can be particularly dangerous for older adults and those with heart disease.
3. Hydration’s Impact on Common Heart Disease Factors
Hydration interacts with several well-known heart disease risk factors, making it a vital consideration in overall heart health management.
3.1 Blood Pressure Regulation
Proper hydration helps maintain blood volume, which supports stable blood pressure. Studies have shown that mild dehydration can lead to elevated blood pressure, a primary risk factor for heart attacks and strokes.
3.2 Cholesterol and Lipid Balance
Water assists in the metabolism and transport of lipids. Dehydration may impair the body’s ability to process fats efficiently, potentially increasing LDL cholesterol levels and accelerating arterial plaque formation.
3.3 Weight Management and Metabolic Health
Staying hydrated can aid in weight control by supporting metabolism and reducing false hunger signals often mistaken for thirst. Since obesity is a major contributor to heart disease, hydration indirectly benefits cardiovascular health through better weight management.
4. Real-Life Stories Demonstrating Hydration’s Role in Heart Disease
Take the example of Mary, a 60-year-old woman diagnosed with hypertension and early signs of coronary artery disease. Initially, Mary struggled with fatigue and high blood pressure despite medication. After consulting her doctor and increasing her daily water intake to at least 2.5 liters, she observed a noticeable drop in blood pressure and improved energy levels within weeks. Her cardiologist attributed this improvement partially to better hydration improving blood volume and vascular function.
Another compelling case is that of Robert, a middle-aged marathon runner who experienced arrhythmia episodes during intense training. By carefully monitoring his hydration status and electrolyte balance, Robert reduced the frequency of these heart irregularities and improved his overall cardiovascular health, highlighting hydration’s critical role even in highly active individuals.
5. Tips to Maintain Adequate Hydration for Heart Health
Adopting a heart-healthy hydration routine involves more than just drinking water; it requires awareness of individual needs and lifestyle factors.
5.1 Drink Regularly Throughout the Day
Aim for consistent fluid intake rather than large amounts infrequently. Sipping water regularly helps maintain steady blood volume and electrolyte balance.
5.2 Recognize Thirst and Early Signs of Dehydration
Pay attention to subtle cues such as dry mouth, fatigue, dizziness, or dark-colored urine. Addressing these signs early prevents cardiovascular strain.
5.3 Balance Electrolytes
Incorporate sources of potassium, magnesium, and sodium as needed, especially during heavy sweating or illness, to maintain heart rhythm stability.
5.4 Adjust Hydration Based on Activity and Environment
Hot weather and physical exertion increase water needs. Customize hydration to fit these conditions for optimal cardiovascular support.
5.5 Avoid Excessive Caffeine and Alcohol
Both can contribute to dehydration and negatively impact heart health if consumed in excess.
6. Resources from HeartCare Hub for Heart-Healthy Hydration
For those looking to optimize heart health through proper hydration, HeartCare Hub offers an array of carefully selected products and expert advice. Whether you need hydration tracking tools, electrolyte supplements, or tailored nutrition plans, HeartCare Hub provides trusted recommendations to support your cardiovascular journey.
Combining proper hydration practices with professional resources from HeartCare Hub ensures a comprehensive approach to managing and preventing heart disease effectively.



















Deborah Heart and Lung Center
deborah heart and lung center
200 Trenton Rd, Browns Mills, NJ 08015, USA