- Heart-Disease-Overview
- Role-of-Blood-Thinning-Medications
- Types-of-Blood-Thinning-Medications
- Managing-Risks-and-Benefits
- Real-Life-Examples-and-Insights
- Finding-Support-and-Resources
1. Understanding Heart Disease and Its Impact
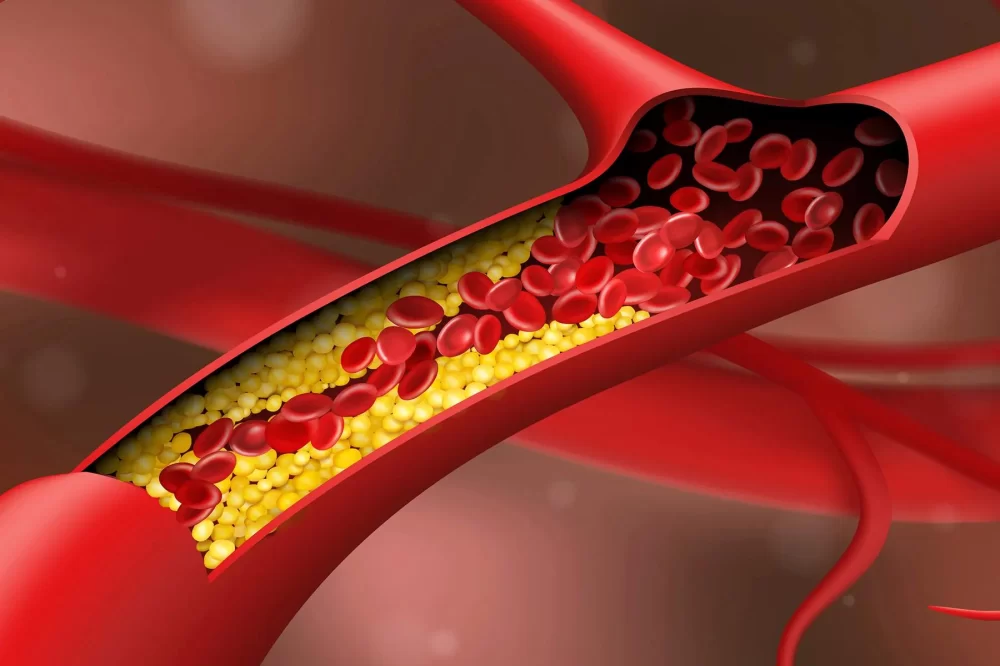
Heart disease remains one of the leading causes of death worldwide, affecting millions of people every year. It encompasses various conditions that impair the heart’s ability to pump blood effectively, including coronary artery disease, heart attacks, and arrhythmias. Central to many heart conditions is the formation of blood clots, which can obstruct blood flow and trigger life-threatening events such as strokes or myocardial infarctions.
What makes heart disease particularly challenging is its silent progression—many individuals do not recognize symptoms until a serious complication occurs. This underlines the importance of proactive management strategies, where blood thinning medications often play a pivotal role.

1.1 The Link Between Blood Clots and Heart Disease
Blood clots are natural responses to injury but can become dangerous when they form inside blood vessels without a clear cause. In heart disease patients, especially those with atrial fibrillation or artificial heart valves, the risk of abnormal clot formation increases significantly. These clots can travel to the brain, causing strokes, or block coronary arteries, leading to heart attacks.
Atlanta Heart Specialists
atlanta heart specialists
4375 Johns Creek Pkwy #350, Suwanee, GA 30024, USA

2. The Crucial Role of Blood Thinning Medications
Blood thinning medications, also known as anticoagulants, are designed to reduce the blood’s ability to clot. Their main objective is to prevent harmful clots from forming while balancing the risk of excessive bleeding. For patients with heart disease, these medications can be lifesaving, significantly lowering the risk of stroke and other complications.
These medications do not "thin" the blood in a literal sense but interfere with the chemical processes that cause clotting. This subtlety is essential to understand for effective treatment and patient safety.
2.1 How Anticoagulants Work
Anticoagulants target specific proteins in the blood clotting cascade. For example, warfarin inhibits vitamin K, which is vital for clot formation. Newer agents like direct oral anticoagulants (DOACs) target thrombin or factor Xa, key enzymes in clot development. This precision allows tailored therapies with varying effects and side effect profiles.
3. Exploring Different Blood Thinning Medications
The landscape of blood thinning medications has evolved over decades, offering patients and clinicians multiple options:
3.1 Warfarin: The Traditional Anticoagulant
Warfarin has been a cornerstone in anticoagulation therapy for over 60 years. While effective, it requires regular blood monitoring and dietary considerations due to its interactions with vitamin K-rich foods and other medications.
3.2 Direct Oral Anticoagulants (DOACs)
DOACs such as apixaban, rivaroxaban, and dabigatran have revolutionized blood thinning therapy. They offer fixed dosing and fewer interactions, improving convenience and adherence. However, they are not suitable for all patients, and cost can be a limiting factor.
3.3 Antiplatelet Agents
Although not traditional blood thinners, medications like aspirin reduce platelet aggregation, an important step in clot formation. These are often prescribed alongside anticoagulants in certain heart disease contexts.
4. Balancing the Benefits and Risks of Blood Thinning Therapy
While blood thinning medications are essential for preventing dangerous clots, they carry an inherent risk of bleeding. Managing this delicate balance requires careful clinical judgment and patient education.
4.1 Monitoring and Lifestyle Adjustments
Regular blood tests and adherence to dosing schedules are critical, especially with warfarin therapy. Patients should be aware of signs of bleeding, such as unusual bruising or blood in urine, and report them promptly. Lifestyle factors, including diet and alcohol intake, also influence medication effectiveness.
4.2 Personalized Treatment Plans
Each patient's medical history, other medications, and lifestyle factors guide the choice of anticoagulant. Some may benefit from newer agents, while others require traditional therapies with close supervision.
5. Real-Life Examples: Stories from Patients and Medical Insights
Consider the story of James, a 68-year-old man diagnosed with atrial fibrillation. Before starting blood thinning therapy, James experienced a minor stroke that severely impacted his mobility. After being prescribed a DOAC and making lifestyle changes, James’s stroke risk dropped dramatically, and he regained independence.
This example underscores the power of anticoagulation in real-world scenarios and highlights the importance of timely intervention.
5.1 Professional Perspectives on Blood Thinning
Cardiologists emphasize that patient education is as important as medication. Understanding the purpose and risks helps patients stay committed to their treatment, reducing complications and hospital readmissions.
6. Accessing Resources and Support for Heart Disease Management
Managing heart disease with blood thinning medications is a journey requiring support and reliable information. Platforms like HeartCare Hub offer valuable resources, including expert advice, product recommendations, and connections to specialized services. For anyone navigating anticoagulant therapy, such support can improve outcomes and quality of life.
In conclusion, understanding the interplay between heart disease and blood thinning medications empowers patients to take control of their health. With the right knowledge and support, risks can be managed effectively, and life can continue with confidence.




















Deborah Heart and Lung Center
deborah heart and lung center
200 Trenton Rd, Browns Mills, NJ 08015, USA