- what-personalized-medicine-means-in-cardiology
- genetics-and-its-role-in-tailored-cardiac-care
- real-world-example-when-one-size-does-not-fit-all
- how-personalized-medicine-improves-outcomes
- getting-started-with-personalized-heart-care
1. What Personalized Medicine Means in Cardiology
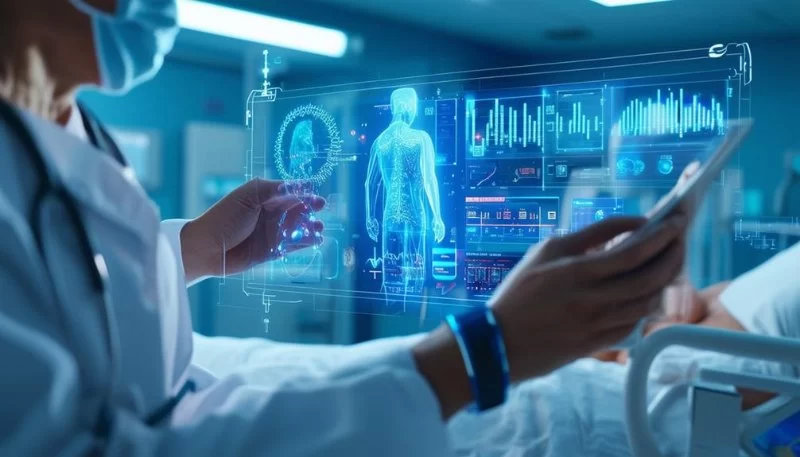
Personalized medicine in cardiology is no longer a distant dream—it’s a present-day reality. Instead of using broad, generalized treatments for heart disease, this approach focuses on tailoring care to the individual. By integrating your genetic information, lifestyle, environmental exposures, and clinical history, cardiologists can make more accurate diagnoses and prescribe treatments that are more likely to succeed.
Imagine walking into a clinic and receiving a heart health plan specifically designed for you—not for someone with “similar symptoms,” but for your unique biological blueprint. That’s the promise of precision cardiology.

2. Genetics and Its Role in Tailored Cardiac Care
2.1 Why DNA Matters
Our genes influence everything from how we metabolize medications to our predisposition for conditions like hypertension or arrhythmias. In personalized medicine, genetic testing can reveal important mutations—like those in the PCSK9 gene—that can inform aggressive cholesterol-lowering strategies or early interventions.
Heartland Cardiovascular Center
heartland cardiology
Madison Medical Plaza, 301 N Madison St # 207, Joliet, IL 60435, USA

2.2 Pharmacogenomics: Matching Medicine to Your Biology
Some patients respond poorly to commonly prescribed heart medications like beta-blockers or statins due to genetic variations. Personalized cardiology uses pharmacogenomic testing to avoid trial-and-error prescribing, reducing side effects and improving therapeutic outcomes.
3. Real-World Example: When One Size Does Not Fit All
Take Sarah, a 52-year-old woman diagnosed with atrial fibrillation. Standard treatment would have been warfarin, but a pharmacogenetic test revealed she would likely metabolize it too slowly—risking bleeding. Her cardiologist at HeartCare Hub switched her to a direct oral anticoagulant (DOAC), which worked better and safer.
This is personalized medicine in action: real data driving real decisions with real-life impact.
4. How Personalized Medicine Improves Outcomes
4.1 Early Risk Detection
Before symptoms arise, genetic screenings can identify risks such as familial hypercholesterolemia or inherited cardiomyopathies. This allows for earlier interventions—sometimes even before damage begins.
4.2 Targeted Therapies for Complex Conditions
Patients with heart failure, for example, may benefit from targeted treatments based on their ejection fraction, comorbidities, and genetic factors. Personalized plans ensure fewer hospitalizations and better quality of life.
4.3 Enhanced Patient Engagement
When patients know their care plan is uniquely designed for them, they’re more likely to stick with it. That leads to better medication adherence, healthier lifestyles, and stronger patient-doctor relationships.
5. Getting Started with Personalized Heart Care
If you're intrigued by the potential of personalized medicine in cardiology, the first step is to find a provider who understands it. Clinics like HeartCare Hub specialize in combining traditional cardiology with advanced diagnostics like gene sequencing, biometric monitoring, and AI-driven predictive modeling.
You might be wondering, “Is personalized care right for me?” The answer is almost always yes—especially if you have a family history of heart issues, are dealing with chronic cardiac conditions, or simply want the most accurate approach available today.
Personalized medicine in cardiology isn't about future possibilities—it’s about transforming today’s outcomes. With advancements in genetic testing, data science, and individualized planning, heart health is no longer guesswork. It’s precision. And it’s personal.




















Monmouth Cardiology Associates, LLC
monmouth cardiology
11 Meridian Rd, Eatontown, NJ 07724, USA