- 1-linking-heart-disease-with-climate-change
- 2-impact-of-air-pollution-on-cardiovascular-health
- 3-extreme-weather-events-and-heart-disease-risks
- 4-vulnerable-populations-facing-greater-risks
- 5-mechanisms-through-which-climate-change-affects-heart-health
- 6-strategies-for-mitigating-risks-and-protecting-heart-health
- 7-real-life-examples-and-heartcare-hub-recommendations
1. Linking Heart Disease with Climate Change
Heart disease remains a leading cause of death worldwide, and emerging evidence highlights the growing influence of climate change on cardiovascular health. Climate change effects such as rising temperatures, increased air pollution, and more frequent extreme weather events contribute to elevated risks of heart-related illnesses. Understanding this connection is critical for public health and personal well-being.
The World Health Organization estimates that environmental factors account for a significant portion of cardiovascular disease burden. As climate change accelerates, its impacts on heart disease are expected to intensify, making it essential to explore how these global shifts influence heart health.

2. Impact of Air Pollution on Cardiovascular Health
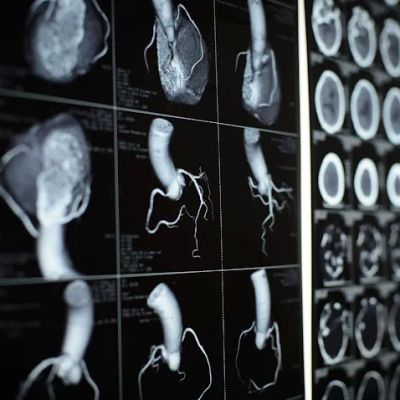
Air pollution is one of the most well-studied climate-related factors affecting heart disease. Fine particulate matter (PM2.5), ozone, and other pollutants exacerbate inflammation and oxidative stress, key contributors to atherosclerosis and hypertension. Long-term exposure to polluted air significantly increases the risk of heart attacks, strokes, and other cardiovascular events.
Studies have shown that cities with higher pollution levels report increased hospital admissions for cardiac conditions. For example, during wildfire seasons intensified by climate change, spikes in air pollution correlate with rises in emergency room visits for heart problems, underscoring the direct health consequences.
Atlanta Heart Specialists
atlanta heart specialists
4375 Johns Creek Pkwy #350, Suwanee, GA 30024, USA

3. Extreme Weather Events and Heart Disease Risks
Climate change leads to more frequent and severe heatwaves, storms, and floods, which place additional strain on individuals with heart disease. Heatwaves increase the risk of dehydration, heat exhaustion, and heart attacks, particularly in vulnerable populations.
Extreme cold spells can also impact cardiovascular health by causing blood vessel constriction and raising blood pressure. Furthermore, disasters disrupt healthcare access and medication supplies, increasing risks of complications among heart patients.
The 2020 California wildfires, fueled by climate change, offer a case study where increased emergency calls for cardiac events were documented during and after the disaster, highlighting the intersection of environment and heart health.
4. Vulnerable Populations Facing Greater Risks
Not all individuals are affected equally by climate change’s cardiovascular impacts. Older adults, people with pre-existing heart conditions, low-income communities, and those living in urban heat islands are disproportionately at risk. Social determinants such as limited access to healthcare and safe housing exacerbate these vulnerabilities.
Health disparities widen as climate change continues, necessitating targeted interventions to protect those most susceptible. Community-based programs that improve awareness and resilience are critical in mitigating these risks.
5. Mechanisms Through Which Climate Change Affects Heart Health
Climate change affects heart disease through multiple interrelated biological and social mechanisms. Environmental stressors like pollution and temperature extremes induce systemic inflammation and autonomic nervous system imbalances. These biological responses increase the risk of arrhythmias, hypertension, and vascular damage.
Additionally, climate-induced disruptions to food security, physical activity patterns, and mental health indirectly impact cardiovascular health. Anxiety related to climate events, disrupted sleep, and altered lifestyle habits further compound heart disease risk.
6. Strategies for Mitigating Risks and Protecting Heart Health
Addressing the nexus of heart disease and climate change requires integrated approaches. Public health initiatives must emphasize reducing air pollution, improving urban green spaces, and preparing healthcare systems for climate-related emergencies.
On an individual level, people can reduce exposure by monitoring air quality, avoiding outdoor activities during extreme weather, and managing heart conditions proactively with their healthcare providers. Promoting clean energy and sustainable policies benefits cardiovascular health at a population level.
7. Real-Life Examples and HeartCare Hub Recommendations
A recent example is the European heatwave of 2019, linked to increased cardiovascular mortality across multiple countries. Public health responses included heat alerts and community outreach programs focused on heart patients, illustrating proactive risk management.
HeartCare Hub recommends routine cardiovascular screenings for those in high-risk areas and offers resources for adapting heart care to a changing climate. Our platform also connects users with trusted products and services designed to support heart health in the face of environmental challenges.
Understanding the interplay between heart disease and climate change effects empowers individuals and communities to act effectively, improving resilience and health outcomes now and in the future.




















Deborah Heart and Lung Center
deborah heart and lung center
200 Trenton Rd, Browns Mills, NJ 08015, USA