- The-Connection-Between-Heart-Disease-And-Anxiety
- How-Anxiety-Affects-Cardiac-Function
- Shared-Risk-Factors
- Recognizing-Anxiety-In-Cardiac-Patients
- Managing-Anxiety-To-Protect-Heart-Health
- When-To-Seek-Professional-Help
1. The Connection Between Heart Disease and Anxiety
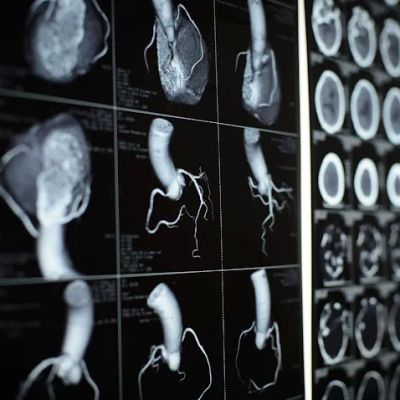
Heart disease and anxiety: understanding the link begins with recognizing that both conditions share an intricate, bidirectional relationship. Anxiety isn’t just a mental health issue—it triggers physiological responses that strain the cardiovascular system. When a person experiences anxiety, the body enters a fight-or-flight state, releasing adrenaline and cortisol. These stress hormones increase heart rate and blood pressure, causing coronary arteries to constrict and limiting oxygen flow. Over time, repeated surges in stress hormones contribute to arterial inflammation and plaque buildup, laying the groundwork for heart disease.
Conversely, living with a diagnosis of coronary artery disease, heart failure, or after a heart attack can provoke persistent anxiety. Patients frequently report fear of another cardiac event, leading to chronic hypervigilance, disrupted sleep, and avoidance of physical activity. This state, sometimes called “cardiac anxiety,” perpetuates the stress response, further burdening an already compromised heart. Research indicates that approximately 30–50% of cardiac patients experience clinically significant anxiety symptoms, which correlate with poorer outcomes and higher mortality rates.
At HeartCare Hub, we emphasize that addressing both heart disease and anxiety requires integrated care. A patient-centered approach includes routine screening for anxiety in cardiology clinics and collaboration between cardiologists, psychologists, and primary care providers. By understanding and treating anxiety alongside heart disease, patients gain better quality of life, improved adherence to cardiac therapies, and reduced risk of recurrent events. This article will explore mechanisms, shared risk factors, signs to watch for, and effective strategies to manage anxiety for optimal heart health.

2. How Anxiety Affects Cardiac Function
Anxiety can be measured not only by racing thoughts and restlessness, but also by concrete changes in cardiovascular physiology. When an anxious episode occurs, the sympathetic nervous system spikes, elevating heart rate (tachycardia) and tightening blood vessels. This acute response may be protective in the short term, but if anxiety becomes chronic, the heart endures persistently elevated workloads. Over months or years, this can lead to hypertrophy of the left ventricle, reduced ejection fraction, and eventually heart failure.
Moreover, anxiety alters heart rate variability (HRV), a marker of autonomic balance. Low HRV signals dominance of the sympathetic “fight-or-flight” system over the parasympathetic “rest-and-digest” system. Studies demonstrate that individuals with both heart disease and anxiety exhibit lower HRV, which predicts higher rates of arrhythmias and sudden cardiac death. Anxiety also promotes unhealthy behaviors—poor sleep, smoking, overeating—that amplify cardiovascular risk.
For example, in one clinical trial, patients with generalized anxiety disorder had a 25% higher incidence of atrial fibrillation over five years compared to controls. Animal studies confirm that elevated cortisol disrupts endothelial function, impairing the ability of vessels to dilate in response to increased demand. Understanding these pathways underscores why heart disease and anxiety: understanding the link is critical for preventing progressive heart damage. Incorporating stress-reduction techniques can rebalance autonomic tone, protect cardiac function, and improve long-term prognosis.
Deborah Heart and Lung Center
deborah heart and lung center
200 Trenton Rd, Browns Mills, NJ 08015, USA

3. Shared Risk Factors
Heart disease and anxiety share multiple risk factors, magnifying the importance of holistic prevention. Lifestyle elements such as sedentary behavior, poor diet, and inadequate sleep contribute to both conditions. Physical inactivity increases the likelihood of obesity, hypertension, and dyslipidemia—key drivers of atherosclerosis—while also failing to provide the natural anxiety relief that exercise offers through endorphin release.
Dietary patterns high in refined sugars and trans fats promote systemic inflammation, fueling both depression and anxiety disorders. These diets also accelerate plaque formation in coronary arteries. In contrast, heart-healthy diets rich in omega-3 fatty acids, antioxidants, and fiber correlate with lower rates of anxiety and improved endothelial health. Smoking and excessive alcohol use present another overlapping risk: nicotine acutely raises blood pressure and heart rate, and chronic smoke exposure accelerates arterial damage. Alcohol, a depressant, can worsen anxiety over time and contributes to hypertension.
Genetic predisposition also plays a role. Variants in genes regulating the hypothalamic-pituitary-adrenal axis can increase susceptibility to both panic disorder and hypertension. Family histories of anxiety disorders and cardiovascular disease often coexist. Awareness of these shared risk factors enables targeted interventions: patients can adopt heart-healthy and mood-stabilizing lifestyles simultaneously, addressing the heart disease and anxiety link at its roots.
4. Recognizing Anxiety in Cardiac Patients
Because symptoms of heart disease and anxiety overlap—chest tightness, palpitations, shortness of breath—patients and clinicians must distinguish between ischemic events and panic attacks. A key difference lies in the onset and duration: panic typically peaks within minutes and resolves, while angina may persist or worsen with exertion. Yet 40% of patients presenting to emergency departments with chest pain receive a diagnosis of panic disorder rather than a cardiac event.
Effective screening includes validated tools like the Hospital Anxiety and Depression Scale (HADS) and the Generalized Anxiety Disorder 7-item (GAD-7) questionnaire. Incorporating these brief assessments into cardiology visits identifies those in need of mental health referral. Patients might describe feelings of impending doom or catastrophic thoughts about heart failure. A collaborative care model ensures that these psychological symptoms are not ignored—they should be managed alongside cardiac medications and lifestyle changes.
Case in point: John, a 58-year-old heart attack survivor, developed severe anxiety about exercising, fearing another event. His ejection fraction improved over months, but his quality of life remained poor until his cardiologist introduced cognitive-behavioral therapy focused on exercise desensitization. By learning to reinterpret chest sensations and gradually increasing activity under supervision, John regained confidence—and his anxiety diminished, aiding his cardiac recovery.
5. Managing Anxiety to Protect Heart Health
Integrative strategies for heart disease and anxiety: understanding the link leads to combined interventions. First-line approaches include lifestyle modifications—regular moderate exercise, a Mediterranean-style diet, and consistent sleep hygiene. Exercise programs should be tailored with cardiac rehabilitation teams to ensure safety and gradual progression.
Mind-body therapies yield significant benefits. Mindfulness meditation reduces cortisol levels and improves HRV, while progressive muscle relaxation alleviates sympathetic overdrive. Studies show that a 12-week mindfulness-based stress reduction program lowered systolic blood pressure by an average of 5 mmHg in hypertensive patients with anxiety. Similarly, yoga combines physical postures with breath control, fostering parasympathetic activation and reducing both anxiety scores and inflammatory markers.
Pharmacologic options may include selective serotonin reuptake inhibitors (SSRIs), which are safe in most cardiac populations, and certain beta-blockers, which both manage heart rate and anxiety-induced palpitations. Close coordination between psychiatrists and cardiologists ensures that medication choices respect cardiac function. For personalized support and resources, HeartCare Hub offers professional consultations, guided mindfulness recordings, and community forums where patients share success stories and tips for managing anxiety while living with heart disease.
6. When To Seek Professional Help
While self-care strategies benefit many, some patients require specialized mental health services. Indicators include persistent panic attacks, debilitating worry, or depressive symptoms interfering with daily functioning. A referral to a clinical psychologist for cognitive-behavioral therapy or to a psychiatrist for medication management may be appropriate.
In severe cases, such as post-traumatic stress after a cardiac arrest, trauma-focused therapies like EMDR (Eye Movement Desensitization and Reprocessing) can address underlying distress. Support groups—either in person or through HeartCare Hub’s online network—provide peer validation and coping strategies. Regular follow-up appointments should monitor both cardiac metrics (blood pressure, lipid profile, ejection fraction) and anxiety levels, adjusting treatment plans dynamically.
Ultimately, heart disease and anxiety: understanding the link empowers patients and providers to pursue comprehensive care. By recognizing signs early, reducing modifiable risks, and integrating behavioral health into cardiology, individuals can not only prolong life but enhance its quality—feeling less fearful and more in control of both their heart and mind.



















Hoag Urgent Care Irvine - Sand Canyon
hoag urgent care
16205 Sand Canyon Ave Suite 100, Irvine, CA 92618, USA