- Understanding Heart Failure and Its Causes
- Medical Treatments for Heart Failure
- Lifestyle Changes for Heart Failure Management
- Advanced Therapy Options for Heart Failure
- Real-Life Case Studies in Heart Failure Treatment
Understanding Heart Failure and Its Causes
Heart failure is a condition where the heart is unable to pump blood efficiently, leading to reduced oxygen and nutrients being delivered to the body’s organs and tissues. This condition affects millions of people worldwide and can be caused by various factors, including coronary artery disease, high blood pressure, diabetes, and heart valve problems.
Understanding heart failure and its underlying causes is crucial for selecting the right treatment options. By addressing the root cause, doctors can help manage symptoms, improve quality of life, and slow the progression of the disease. In this article, we will explore the most common treatment options available for heart failure and how they can benefit patients.

Medical Treatments for Heart Failure
Medical treatments for heart failure primarily focus on relieving symptoms, preventing further damage to the heart, and improving overall heart function. There are several medications and therapies that are commonly prescribed to patients with heart failure:
1. ACE Inhibitors and ARBs: Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) help relax blood vessels, reduce blood pressure, and improve blood flow to the heart. These medications are crucial in treating heart failure by reducing the heart's workload.
2. Beta-Blockers: Beta-blockers work by slowing down the heart rate and reducing blood pressure. These medications help prevent the heart from working too hard and can improve heart function over time.
3. Diuretics: Diuretics, also known as water pills, help reduce fluid buildup in the body, which is a common issue for heart failure patients. They assist in relieving symptoms like swelling and shortness of breath.
4. Aldosterone Antagonists: These medications help regulate the balance of salt and fluid in the body, preventing fluid retention and reducing strain on the heart.
5. Inotropes: In some cases, patients may be prescribed inotropic medications, which help increase the heart's pumping ability, particularly in advanced stages of heart failure.
Atlanta Heart Specialists
atlanta heart specialists
4375 Johns Creek Pkwy #350, Suwanee, GA 30024, USA

Lifestyle Changes for Heart Failure Management
While medications are essential in managing heart failure, lifestyle changes play a crucial role in improving heart health and overall well-being. Here are some key lifestyle modifications for heart failure patients:
1. Dietary Adjustments: A heart-healthy diet is essential for managing heart failure. Reducing salt intake can help prevent fluid retention, while eating more fruits, vegetables, and whole grains can improve heart function. Limiting alcohol and caffeine is also advised to prevent strain on the heart.
2. Regular Exercise: While it may seem counterintuitive, light physical activity is important for heart failure patients. Exercise can help improve circulation, reduce stress on the heart, and enhance overall cardiovascular health. Always consult a healthcare provider before starting an exercise program.
3. Weight Management: Maintaining a healthy weight is essential for reducing the strain on the heart. Excess weight can worsen heart failure symptoms and contribute to other health issues like diabetes and high blood pressure.
4. Stress Management: Chronic stress can exacerbate heart failure symptoms. Practicing relaxation techniques like deep breathing, meditation, and yoga can help reduce stress levels and improve heart health.
Advanced Therapy Options for Heart Failure
In more severe cases of heart failure, advanced therapy options may be considered to help improve heart function and prolong life. These treatments are typically recommended when other treatments are no longer effective:
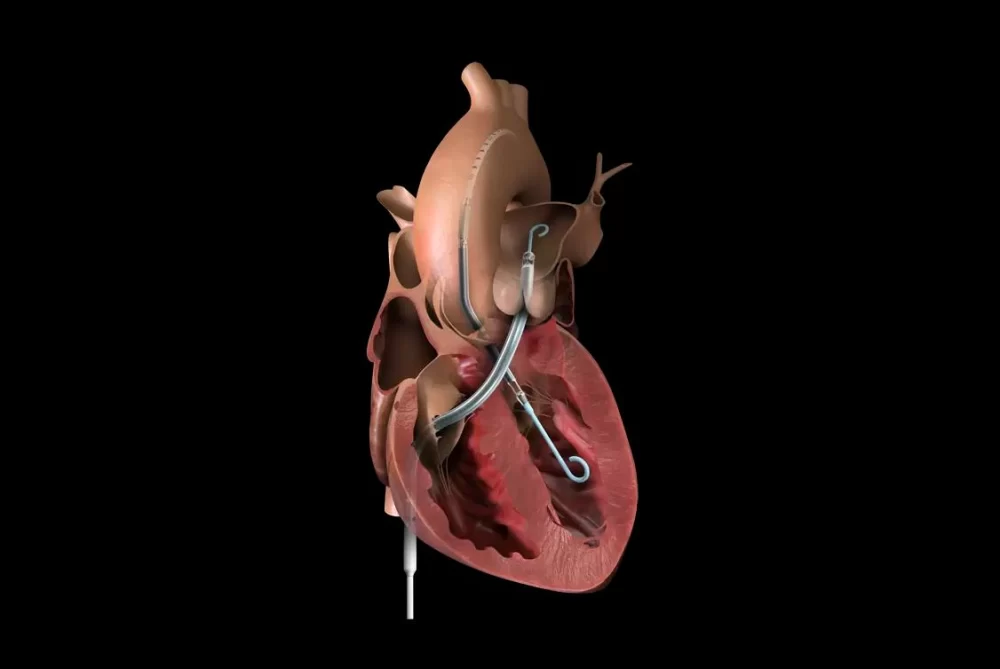
1. Implantable Cardioverter Defibrillators (ICD): An ICD is a device that monitors the heart's rhythm and can deliver shocks if it detects life-threatening arrhythmias. It is particularly useful for patients with heart failure who are at risk of sudden cardiac arrest.
2. Cardiac Resynchronization Therapy (CRT): This therapy involves implanting a special pacemaker to help the heart's chambers beat in sync. CRT can improve heart function, reduce symptoms, and enhance the quality of life for heart failure patients.
3. Heart Transplantation: In cases of end-stage heart failure, a heart transplant may be necessary. This is typically considered when other treatments have failed, and the patient's heart can no longer function effectively.
Real-Life Case Studies in Heart Failure Treatment
Consider the story of Sarah, a 62-year-old woman diagnosed with heart failure after years of uncontrolled high blood pressure. Initially, Sarah struggled with symptoms like shortness of breath, swelling, and fatigue. After consulting her doctor, she was prescribed a combination of ACE inhibitors, beta-blockers, and diuretics to manage her symptoms.
Sarah also made significant lifestyle changes, such as reducing her salt intake, increasing her physical activity, and managing her stress levels. Over time, she noticed an improvement in her energy levels and a reduction in fluid retention. As her condition progressed, Sarah’s doctors recommended she undergo CRT, which further improved her heart's function and allowed her to maintain a good quality of life.
Real-life stories like Sarah’s show that heart failure can be effectively managed with a combination of medications, lifestyle changes, and advanced therapies. If you or a loved one are facing heart failure, visit HeartCare Hub for the best heart care products and services to support your journey toward better heart health.





















Deborah Heart and Lung Center
deborah heart and lung center
200 Trenton Rd, Browns Mills, NJ 08015, USA